Image

Telemedicine visit with Kaiser Permanente.
|
COURTESY OF KAISER PERMANENTE NORTHWEST
Image

Abortion pills.
|
PHOTO BY VALASIURUA/WIKI COMMONS
Image

Telemedicine visit with Kaiser Permanente.
|
COURTESY OF KAISER PERMANENTE NORTHWEST
Image
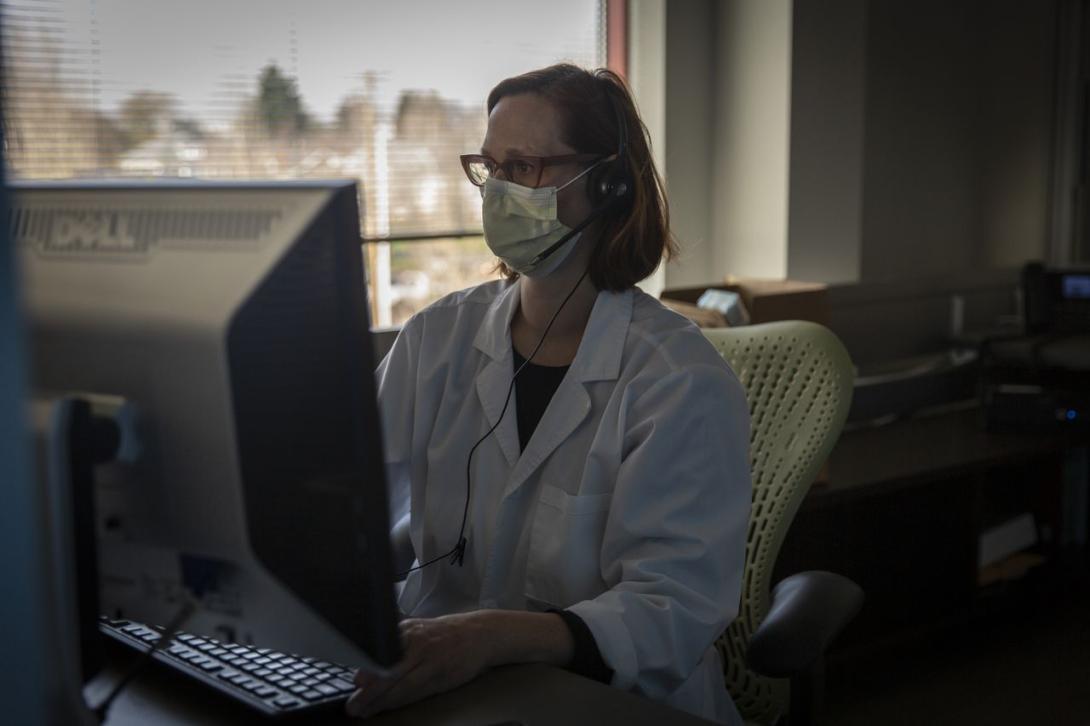
Dr. Paula Bednarek works at her computer in the Planned Parenthood Northeast Portland Health Center.
|
BROOKE HERBERT/THE OREGONIAN/OREGONLIVE
Image

Telemedicine visit with Kaiser Permanente.
|
COURTESY OF KAISER PERMANENTE NORTHWEST
Image

Telemedicine visit with Kaiser Permanente.
|
COURTESY OF KAISER PERMANENTE NORTHWEST
Image

Telemedicine visit with Kaiser Permanente.
|
COURTESY OF KAISER PERMANENTE NORTHWEST