Patients in Eugene and Springfield are experiencing delays for emergency care as ambulances are forced to travel greater distances in the wake of PeaceHealth’s closure of the only emergency department in Oregon’s third-largest city.
Patients who used to be served in the emergency room of the now-shuttered University District hospital in Eugene instead need ambulances to take them six miles away to PeaceHealth’s RiverBend hospital in Springfield. That translates to about a half-hour longer for ambulances to transport these patients to an emergency room, Chris Heppel, deputy chief of Eugene Springfield Fire, told The Lund Report.
“It’s taking our time away,” said Heppel, of the added travel distance and delays transferring patients at the hospital, which he said is time ambulances could be answering other calls. His agency is the largest government-run ambulance service in the state.
The situation caused by the closure has caught the attention of State Rep. Nancy Nathanson, D-Eugene. She’s spearheading a bill to cut down on delays and improve patients’ chances of survival. House Bill 4136 would provide $4.5 million to temporarily staff an additional ambulance through June 2025 while funding pilot programs directing patients with less urgent needs away from overburdened emergency departments.
A proposed amendment to the bill specifies that $1.3 million of that amount would go toward additional ambulance services and $3.2 million for the pilot program.
The legislation is intended to provide relief to patients who have sometimes had to wait hours in ambulances to be transferred to the RiverBend emergency room, Nathanson told The Lund Report. She also said the bill seeks to improve upon the health care system.
“We don’t want to rebuild the same old system that wasn’t working,” she said. “We need to look toward the future.”
In a text to The Lund Report, Laurie Trieger, a member of the Lane County Board of Commissioners, praised Nathanson and said the bill “will help mitigate some of the impacts of losing local emergency medicine capacity in a way that will also help other communities around Oregon who are likewise struggling to ensure emergency room access.”
But in the meantime, the Eugene hospital’s closure is contributing to patient care delays and putting pressure on the area’s emergency medical system.
Regionwide impact
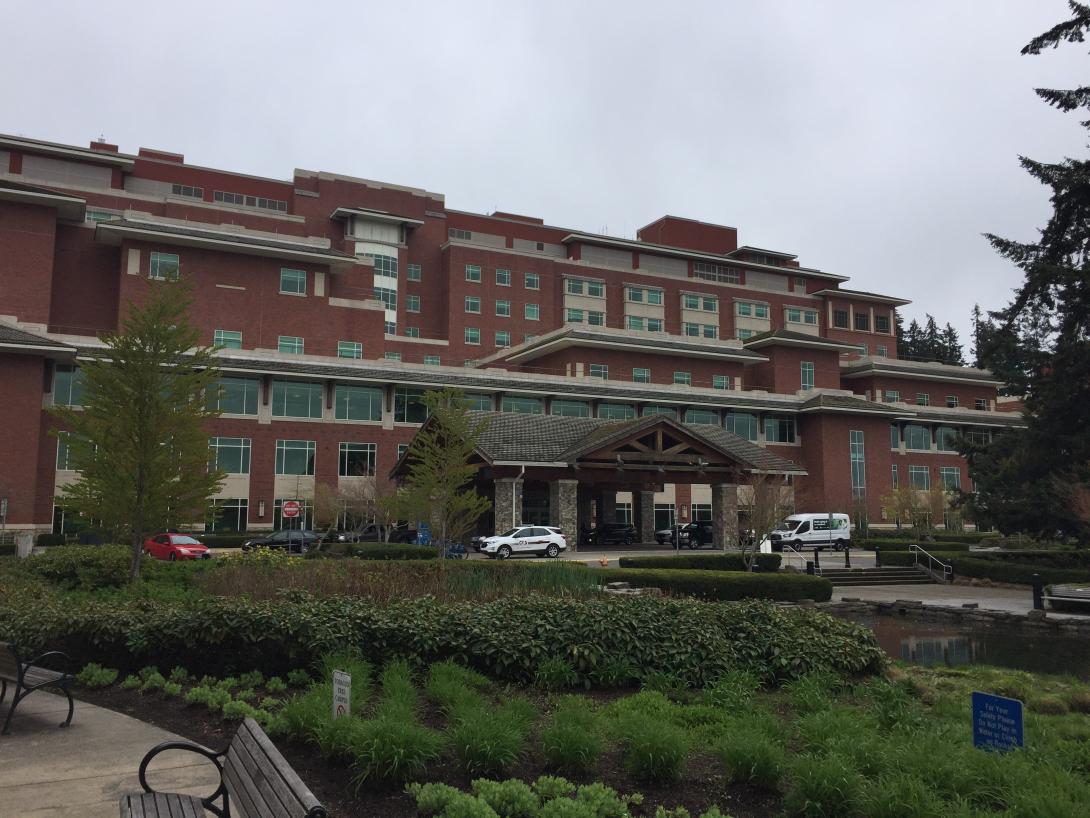
Vancouver, Washington-based PeaceHealth announced in August that it would close its University District hospital in Eugene in response to financial losses and a decline in its use. Despite pushback from the community and Gov. Tina Kotek for PeaceHealth to change course, it moved forward with the hospital closure in December. The loss of the hospital has forced the area’s emergency responders into a balancing act of managing resources.
Heppel said University of Oregon students who previously would have walked to the University District emergency department are now directed to Riverbend.
CAHOOTS, Eugene’s mobile crisis intervention service, is also taking its patients to RiverBend or McKenzie-Willamette Medical Center, even farther away in Springfield, he said.
“It’s a systemic impact, not just fire and EMS,” he said. “We’re driving farther and taking longer to get patients off the gurney.”
Before the closure, RiverBend already had the highest wait time in the area between when an ambulance brought a patient to the hospital and when they were transferred to its emergency department. Heppel said wait times have been increasing for years. Patients are now sometimes waiting half an hour to an hour and a half on hospital gurneys before being taken into a hospital, he said.
Eugene Springfield Fire figures show that in December 2022, patients waited a total of 222 hours in ambulances parked at RiverBend before being taken in by its emergency department. For the University District, that number was 77 hours, and it was 74 hours for McKenzie-Willamette Medical Center, which is owned by Tennessee-based corporation Quorum Health Corp. A year later and after the University District closure, RiverBend’s time waited increased to a cumulative 292 hours. McKenzie-Willamette shot up to 132 hours.
The average time patients spent waiting in ambulances to be transferred to hospitals has also increased for the area, according to agency figures. In January 2024, the average wait time rose to roughly 17 minutes from 11 minutes a year ago. The longest wait times increased from 22 minutes to 38 during that period. The number of transports during that time stayed nearly flat, rising by roughly 100 to 1,842 in January 2024.
While waiting for a patient to be accepted at the emergency room, Heppel said an ambulance isn’t out taking calls in Eugene Springfield Fire’s large service area because its crew stays with the patient.
Heppel said Eugene Springfield Fire serves about 380,000 people in a coverage area that extends beyond the two cities into communities on the McKenzie Highway.
Eugene Springfield Fire runs seven advanced life support ambulances 24-hours a day, in addition to three basic life support ambulances during the day and two and night, he said.
The bill would pay for a basic life support ambulance that would run for 12 hours a day and would be staffed by a reserve unit, said Heppel. That won’t solve all the problems caused by the hospital closure, but it would improve the situation until the system stabilizes, he said.
The ‘bowling alley’
RiverBend is a level two trauma center, meaning its 44 private rooms are equipped for any life-threatening situation. McKenzie-Willamette is a step down, with a level three trauma center.
Kevyn Paul, who has worked as a registered nurse for 34 years, told The Lund Report that RiverBend emergency department is significantly busier and more chaotic than the University District hospital where she used to work.
She said the RiverBend emergency department is nicknamed “the bowling alley” because it’s all hallways, which she said make communication between staff more difficult. More patients who don’t need surgery or intensive care — the kind who previously would have gone to University District — are now being sent to RiverBend, she said.
“We have a problem with moving patients out of the emergency department,” she said, adding that patients are now taking up beds in the emergency department for two or three days, boarding there while waiting to be admitted to the hospital.
Paul said she’s watched ambulance crews wait at the RiverBend emergency department for patients to be transferred, and that Nathanson’s bill would help. In the meantime, she worries that the added pressures on the emergency department will mean staff won’t have enough time with patients to spot a serious symptom.
While she realizes it’s impossible, she said it would be better to still have the beds at the University District hospital, which she said was prepared for patients with acute mental illness.
Overused emergency departments
While Nathanson’s bill is focused on a local issue, she said she hopes the second part of the legislation changes health care in communities across the state.
Eve Gray, Lane County’s director of Health and Human Services, told the House health committee last week that after PeaceHealth announced the University District closure Nathanson assembled community leaders to discuss how to protect access to health care.
A consensus emerged from these meetings that the closure would mean gaps in care because local emergency departments are already overwhelmed, she said.
“And yet hospitals were identifying numerous utilizers of the emergency department who did not require a hospital level of care,” she said. “But due to insurance, lack of access to primary care or unmet social needs were ending up in the ED.”
Nathanson said that when someone calls 911 with a medical emergency they are usually taken to the emergency department even if they don’t have a life-threatening condition. They’re left waiting for sometimes hours to get care.
She said the pilot program will focus on these situations and look into less costly options for these patients, like sending a nurse practitioner to their home or taking them to urgent care in a vehicle other than an costly ambulance. Others might be directed to a nurse advice line, she said.
The bill would set up an “innovation fund” overseen by Lane County Public Health that could support “community health care response programs, alternative medical transportation options and programming” that improves access while reducing emergency department visits.
Lane County Public Health would submit reports to lawmakers and the Oregon Health Authority at the end of 2024 and 2025 describing how it spent the innovation fund and possible legislative recommendations.
Ryan said these programs could help, but noted that diverting 911 calls from emergency response can be a challenging task.
“People don’t always know what level of care they need,” she said. “It’s an emergency to them.”