This article was originally published by Oregon Public Broadcasting.
Haylie Helms’s cells are stuck to the side of a clear plastic bottle like thousands of invisible barnacles.
“If you stick them in one of these flasks and give them the right [nutrients], the cells continue to grow and they will spread out on the plastic,” she explains as she starts to tap the bottle with the side of her palm.
The shallow pink liquid in the bottle ripples under the impact. As the cells pull away from the side, the liquid becomes slightly hazy. Helms transfers the solution to a test tube and spins it down in a centrifuge.
When it comes out, the liquid is clear again and there’s a faint whitish smudge in the bottom of the tube.
“So it’s not the easiest to see, but… there’s a little clump there at the bottom,” she says. “There’s about a million cells in that little pellet.”
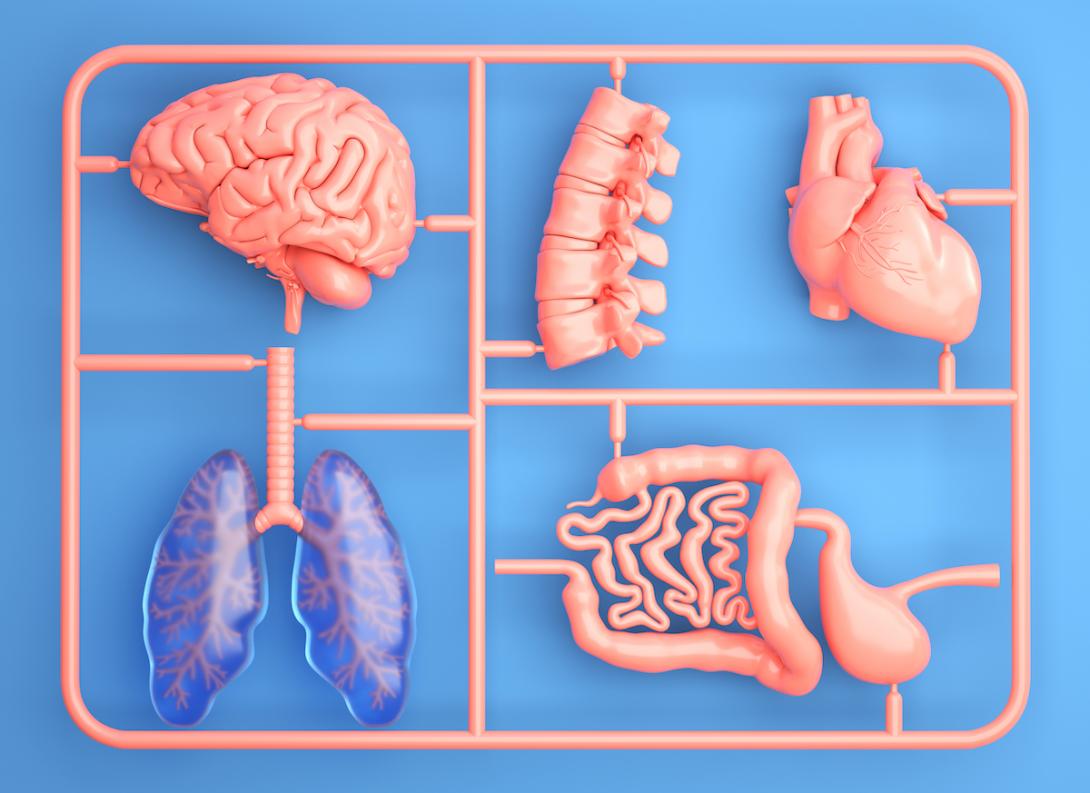
Cells are the tiny building blocks of life, and these cells are key to the Oregon Health and Science University researcher’s cutting-edge work in a medical science field called biofabrication – essentially building with biology. One of the long-term goals for biofabrication is creating transplantable human organs.
Over the course of many months, Helms has developed a way to 3D print individual cells. It’s a technique that may bring the field closer to this goal.
“Kind of like how an inkjet printer works – you have all of your different colors. I can just put different cell types in each of the channels,” she says.
The printer she uses for her work is commercially made, but what she’s doing with it — printing one tiny cell at a time to understand how they interact with each other — is very new.
“I print all types of cells. And the goal is to take all the cells that make up a tissue and put them together in the proper pattern,” she says.
The technique is so new, that when representatives from the printer company visited the Portland lab where Helms works, they were amazed.
“Even when I told the company that this is what I’m doing, they told me that that is not possible. And I said, ‘Please watch,’” she said.

Cancer interactions
Loaded in her printer cartridge on this day are prostate cancer cells.
Helms grabs a video game controller and uses it to move the printer head.
“Move up and down, left, right, and then tell the cells when to come,” she says without taking her eyes off a computer screen that shows a highly magnified image of the printing surface. “Because when what you print is like a fraction of a millimeter, it’s hard to find it later.”
She presses a button, and suddenly a white dot appears against the grey background of her screen.
“This little dot is one individual cell,” she says.
She moves a few microns to the left and deposits another — now two prostate cancer cells placed with incredible precision.
“Everyone teases me that I don’t actually work. I just sit here and play video games all day,” she says.
But the stakes here are much higher than in your average video game.
“It’s not just the genetic mutations within the cancer that caused it [to form]. It’s also how the cells are arranged. If one cell type is next to a different cell type, that can actually indicate if you’re going to have a better or worse prognosis,” Helms says.
Helms is using her printing technique to figure out how different configurations of cells behave.
“I will take a cancer cell and I’ll put healthy cells around and I will see: How do these cells communicate?” she explains. “Does the cancer keep growing? Do the healthy cells act more cancerous? And we keep changing the patterns and the cell types to find out: How are these cells talking to each other?”
And ultimately, it may reveal what makes one person’s cancer more aggressive than another’s — and that information is very valuable. Because once they understand the interactions between the cells, researchers have the information they need to develop new treatments.
“[Cancer] drugs are targeting the specific interactions and the mechanisms of how the cells work,” Helms says. “If you don’t know what that mechanism is, you can’t create a drug for it.”
Starting small, thinking big
While Helms’ research focus is currently on cancer, OHSU associate professor Luiz Bertassoni is excited about what could soon be possible because of the new cell-by-cell printing work.
“You know, we’re really laser focused on precision,” he says.
Bertassoni heads up the lab where Helms works.
“Every single cell in your body is there for a reason — quite literally,” he says. “We are particularly interested in replicating that level of precision that nature brings us because we think that that is the key to actually recreating the function that the body has.”
Plainly put, Bertassoni’s goal is to be able to 3D print complex human organs that function in people.
According to the Health Resources and Services Administration, more than 100,000 people in the United States are waiting for organ transplants. Seventeen people waiting for transplants die every day.
Printing transplantable organs is a challenge many labs around the world are tackling. There’s been huge progress in building tissues and simplified versions of organs, but Bertassoni says no one has gotten them to fully function like those in living organisms.
He thinks that being able to precisely replicate an organ — cell by cell by cell — is the way to get over this hump.
Helms’s 3D-printing technique may provide the means to achieve this.
“With the other methods of tissue engineering that are out there, we can create the structures. We can lay down the proteins and the scaffolding that makes the shape,” she says. “But now with this we can also then add in the cells in the arrangement that they need to be.”
Scale and speed
But there’s a lot that needs to happen before being able to create transplantable lab-grown/fabricated organs is possible.
“It is a potentially promising solution. … In principle, that is possible,” says University of Utah engineer Yong Lin Kong, who specializes in biomedical 3D printing, but is not connected to the OHSU work. He has closely tracked developments in the field.
“Of course, there will also always be … unanticipated challenges,” he says. “Because we still have a lot to learn from biology on how cells and tissues come together. And that missing information could be the next hurdle once they have built those systems.”
But even before that, Bertassoni says, the challenges of building something as large as a human organ are considerable. And getting the needed level precision cell construction at a scale that’s meaningful for the human body is a big one.
“You’re able to put three cells close to one another — yeah, that’s cool. That’s important. But can you [place] three or four cells, four million times? Which is really what it would take to build an entire liver,” he says.
And this is the direction the OHSU lab is going.
“This is just the beginning. We’re refining our processes. We’re scaling up. We’re making this quicker, reproducible, says Helms.
Bertassoni acknowledges there’s a long road ahead for precision printing technology. But the implications of this approach for personalized healthcare are nothing short of astounding.
“If you walk into a hospital and say, ‘I have liver failure, I need a new liver,’” Bertassoni says, imagining a scenario in the not-so-distant future.
“[And you say,] ‘Wait a minute, I’m going to print you a liver.’ And you bring a liver that is specific for that patient.. Then, you change medicine forever.”
This story was produced as part of OPB’s science series “All Science. No Fiction.” which focuses on solutions-based research happening in the Pacific Northwest.
Interested in learning more about the incredible biofabrication research happening at OSHU? Enjoy your science in video form? Check out the latest episodes of “All Science. No Fiction.”