Over the past four years, enrollment in Medicaid managed care has increased by 48 percent, with 46 million beneficiaries now receiving coverage through these plans. The government will soon update regulations that direct the plans providing this coverage.
A proposed rule currently at the Office of Management and Budget will update federal regulations from 2002 governing Medicaid managed care organizations (MMCOs). While states have broad flexibility to implement Medicaid, the federal government sets minimum standards for the program and for private plans providing coverage to beneficiaries. Avalere anticipates that the rule will aim to accommodate the evolution of managed care programs and address commonly identified weaknesses. Among other topics, new proposed regulations will likely include additional requirements for plans and states around:
- Medical loss ratio (MLR), including setting a minimum MLR for MMCOs;
- Network adequacy and access to providers, including standards to evaluate provider access and a focus on accuracy of network information provided to beneficiaries;
- Quality measures, including greater standardization of metrics across states and plans, potentially in the form of a star ratings system similar to the one found in Medicare Advantage;
- Actuarial analysis and rate setting, including federal oversight of rate setting and a more detailed, regimented process for ensuring actuarial soundness;
- Continuity of care, including alignment of enrollment practices between Medicaid fee-for-service, MMCOs, and exchange coverage; and
- Public reporting and transparency, including stronger public reporting and transparency requirements for MMCOs and states.
“This will be the first major overhaul of these regulations since 1993. Given the evolution of Medicaid, we expect that changes could be substantial,” said Michael Lutz, director at Avalere. “Greater focus on transparency and oversight could have particular implications for health plans and states.”
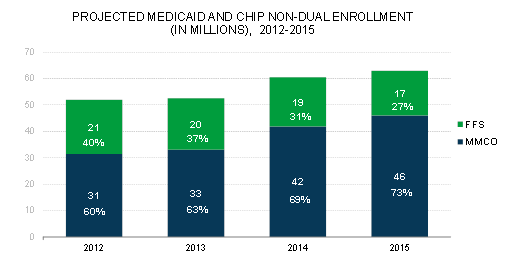
The impact of this regulation could be particularly significant given the size of the beneficiary population affected. States’ use of managed care has grown dramatically in recent years as states have moved more populations from fee-for-service (FFS) to managed care plans and total Medicaid enrollment has grown as a result of the Affordable Care Act. By the end of 2015, Avalere estimates that 73 percent of Medicaid beneficiaries[1] will receive services through MMCOs. (For state-specific numbers, see Table 1.)
Given the extent to which states have expanded their use of managed care, this regulation will have a significant impact,” said Caroline Pearson, senior vice president at Avalere. “MMCOs do not just cover moms and kids anymore—states are now using these plans to cover beneficiaries with complex and chronic conditions, those in rural areas, and many new enrollees under the Affordable Care Act.”
With the expected size and scope of this rule—along with the size of the population affected—states, plans, and other industry stakeholders are eagerly awaiting its arrival. Once the regulation is released, the public will have an opportunity to weigh in on the proposed policy changes during a public comment period.
Methodology
MMCO enrollment projections based on Avalere’s proprietary Medicaid managed care enrollment model. All enrollment numbers exclude dual eligible beneficiaries. Managed care enrollment includes only private plans that are fully capitated for medical services. Avalere assumes the following states opt out of the ACA Medicaid expansion through 2015: AK, AL, FL, GA, ID, KS, LA, ME, MS, MO, MT, NE, NC, OK, SC, SD, TN, TX, UT, VA, WI, and WY. For premium assistance, Avalere assumes AR enrolls all new Medicaid eligibles into the exchange through premium assistance and IA enrolls some new eligibles above 100 percent FPL in premium assistance. Individuals projected to enroll in premium assistance are not counted as Medicaid lives for the purpose of the analysis.
###
To speak with an expert about this analysis, please contact Amy Martin Vogt at [email protected] or 202-745-5052.