A new Avalere analysis finds that participation in the Centers for Medicare & Medicaid Services’ (CMS) voluntary Bundled Payment for Care Improvement (BPCI) program remains strong even after the introduction of downside risk. As of October 1, 2015, 1,500 providers are participating and testing an average of nine unique episodes for a total of about 14,000 clinical episodes. Whereas BPCI’s first phase gave providers free access to new data with no commitment required, beginning in October 2015, CMS requires all participants to accept downside risk for all program bundles. The current participants represent about 25 percent of providers that expressed interest in the program. The decrease in participation raises questions about whether CMS will continue with voluntary demonstrations, such as BPCI, or will move into mandatory programs, such as the Comprehensive Care for Joint Replacement (CJR) program.
“Strong participation in a voluntary program shows providers’ willingness to test new alternative payment models,” said Josh Seidman, senior vice president at Avalere. “However, the fact that many providers that entered the program decided it’s not currently in their financial interest to accept downside risk may cause CMS to consider additional mandatory programs in the future.”
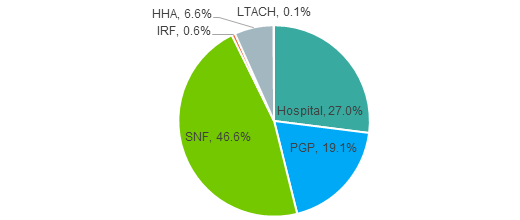
BPCI is a voluntary program in which hospitals, physician group practices and post-acute care providers accept clinical and financial risk for patients over specified time frames. Skilled nursing facilities (SNFs) and hospitals are the most common provider types participating with almost 50 percent and 30 percent of all participants respectively (See Figure 1). Episodes are 30, 60, or 90 days long and providers are responsible for all clinical care provided to the patient over those timeframes. Prior to October 2015, participants could test conditions but not be responsible for spending above the target price. As participants, providers received access to Medicare claims data and target prices allowing them to assess their opportunity under the program. With the requirement for downside risk, many providers determined that BPCI is not the right opportunity for them; however, the experience will help prepare them for future alternative payment models.
CMS allows participating providers to select episodes to test from a group of 48 clinical conditions, which range from procedures (such as joint replacements) to medical conditions (such as sepsis). On average, each participant is testing episodes for nine unique clinical conditions; however, there is considerable variation among participants. While many providers are testing only a few episodes, almost 15 percent of participants are testing more than 20 conditions. The four most commonly tested conditions are lower extremity joint replacement, pneumonia, chronic obstructive pulmonary disease, and congestive heart failure (see Figure 2). These top conditions represent about 18 percent of the 14,000 bundles in the demonstration. The diversity of conditions and participants will provide CMS with substantial information on the impacts of bundled payments as they review the demonstration results.
“The BPCI program serves as an important foundation on which CMS can build toward its goal of shifting 50 percent of Medicare fee-for-service payments to alternative payment models by 2018,” said Erica Breese, manager at Avalere.
Figure 2. Top 10 BPCI Conditions
1. Major joint replacement of the lower extremity
2. Simple pneumonia and respiratory infections
3. Congestive heart failure
4. Chronic obstructive pulmonary disease, bronchitis, asthma
5. Hip & femur procedures except major joint
6. Sepsis
7. Urinary tract infection
8. Acute myocardial infarction
9. Medical non-infectious orthopedic
10. Other respiratory
###
To speak with an expert from Avalere about this new analysis, please contact Frank Walsh at [email protected], or 504-309-5164.
Avalere Health is a strategic advisory company whose core purpose is to create innovative solutions to complex healthcare problems. Based in Washington, D.C., the firm delivers actionable insights, business intelligence tools and custom analytics for leaders in healthcare business and policy. Avalere's experts span 230 staff drawn from Fortune 500 healthcare companies, the federal government (e.g., CMS, OMB, CBO and the Congress), top consultancies and nonprofits. The firm offers deep substance on the full range of healthcare business issues affecting the Fortune 500 healthcare companies. Avalere’s focus on strategy is supported by a rigorous, in-house analytic research group that uses public and private data to generate quantitative insight. Through events, publications and interactive programs, Avalere insights are accessible to a broad range of customers. For more information, visitavalere.com, or follow us on Twitter @avalerehealth.