
Medicaid members have been calling the state’s helpline in recent weeks with questions about new eligibility requirements.
The state has started to verify whether each of the 1.5 million members still qualify now that the COVID emergency is over and extra federal benefits have ended.
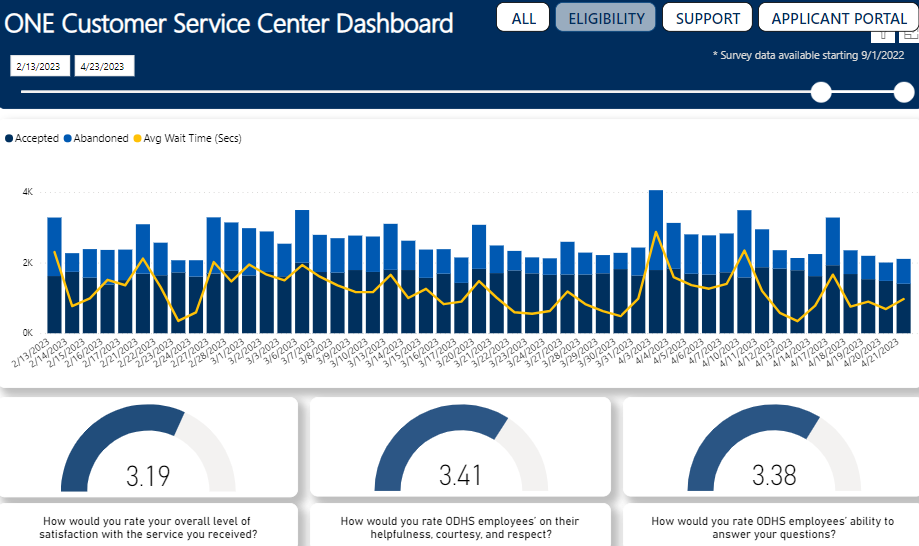
This process started this month, and the state’s helpline is lacking, residents say. Callers always have to wait, sometimes for an average of 15 minutes, sometimes more than an average of 30 minutes, according to the Department of Human Service’s dashboard. It shows that hundreds of callers a day, and sometimes a few thousand, asking about Medicaid and other benefits hang up, apparently fed up with waiting.
Members give the helpline a mediocre score, 3.16 out of 5 for the service in general and 3.39 out of 5 for the call takers’ ability to answer questions. That’s less than the department’s goal, Jake Sunderland, the agency’s press secretary, told the Capital Chronicle in a statement.
“Our service goal is an average satisfaction survey score of four or higher,” Sunderland said.
Even worse: At least one member on the Oregon Health Plan, Oregon’s version of Medicaid, was given misinformation – twice.
“They told me I can’t earn more than about $16,000,” the woman, who requested anonymity, told the Capital Chronicle. “One six months ago told me $18,000.”
Status in April
The Medicaid verification process started this month. The Oregon Health Authority said Monday that it had renewed 140,000 members, requested more information for nearly 47,000 members and notified 6,000 that they will lose coverage.
- To update your information, go to the One system.
- Medicaid members can call 800-699-9075 with questions.
Both figures are wrong. The income limits are based on federal poverty levels, which are updated by the federal government every year. Federal rules limit Medicaid to those earning up to 138% of the federal poverty level, now nearly $19,400 a year for one person, but under a temporary waiver Oregon has extended that to 200%, or about $29,000 a year, for one person.
Sunderland said eligibility status is based on many factors.
“There are many different financial considerations for Medicaid eligibility along with considerations of household composition as well as age and disability statuses and many other factors,” he said. “This makes it incredibly complicated to accurately give ‘salary limit’ information to callers who have general questions and are not seeking to apply or renew benefits.”
Nevertheless, income is a key benchmark, and the salary limits are clear.
Vivian Levy, interim deputy Medicaid director at the Oregon Health Authority, said the misinformation indicates that state officials need to continue training call takers to make sure they have the correct information.
“There’s a tremendous number of changes that are happening right now,” Levy told the Capital Chronicle. “And that requires a lot of training and a lot of communication in a lot of different ways with staff across the state.”
Sunderland said the agency has been preparing for the redetermination process since last fall and has held many training sessions. He said the state is “taking steps” to ensure that call takers have the necessary expertise.
“There are a number of regular opportunities and venues for eligibility staff to request support and ask questions,” Sunderland said. “In the early weeks of this project, we are seeing many case-specific questions and there have not been any broad trends yet in the support our workforce is asking for.”
Even if call takers have wrong information, Medicaid members won’t be kicked off the free medical and dental insurance if they qualify, Levy said. A computer system determines eligibility based on information collected by a data system called the Federal Data Services Hub, which gathers data on citizen, immigration and incarceration status.
To verify income, the state does not use annual tax forms. It relies on Verify Current Income, a service produced by Equifax, the credit-rating company. Levy said the income of many Medicaid members fluctuates, and the verify service has the most accurate monthly figures.
Levy said the state tries to verify as much information as possible and when gaps remain, officials ask members for more information. She said members should ensure that their information is up to date and respond quickly to questions to retain coverage.
If a member doesn’t respond to a request for information, they’ll receive two reminder notices, one after 30 days and one after 60, Levy said. If they still fail to respond, they’ll receive notice after 90 days that their coverage will end in two months.
Members who think the state has made a mistake can appeal, and an administrative law judge will make the final determination, Levy said.
The federal government, which pays for most of Medicaid while the state pays for the rest, regularly audits the state.
“A couple of times a year they actually pull cases out of our system and look at them and make sure that they were determined correctly,” Levy said.
Health authority officials estimate that up to 300,000 people now earn more than 138% of the federal poverty level, but they expect that about 65,000 will retain coverage under the new, temporary income limit of 200% of the federal poverty level.
Levy said the process for Medicaid members – regardless of whether they qualify under the 138% limit or the 200% limit – should be seamless.
Officials are urging members who lose coverage to buy a policy on the federal marketplace, which offers subsidies. Less than 150,000 people in Oregon have purchased marketplace coverage, and a majority qualify for subsidies.
Levy said the state hopes Oregon’s uninsured rate stays the same – about 5% of Oregonians lack health insurance. But it’s unlikely that everyone who loses their Medicaid coverage will purchase a plan.
The Oregon Health Authority expects it will take months to determine the status of all members.

If we had publicly funded healthcare also known as singlepayer none of this would be necessary. These are people not numbers. I would like to know how much it costs to administer this system. Whatever it costs is wasted money. Also the health providers, like Doctors, Nurses, Dentists, Clinics are getting paid less than Medicare amounts. We need to move to a system that provides healthcare to everybody.