Since the 1990s, the cost of medical care has seen the greatest rate of inflation across all sectors, suppressing wages and limiting economic growth. The system is an enormously complicated technical approach to a complex problem. But complicated is not complex, and only complexity can manage complexity; working harder at the old paradigm won’t yield a different outcome.
It doesn’t need to be this way. Since the turn of the century, the businesses that have dominated their industries take advantage of complexity through network models , allowing them to:
- Focus on purpose, separating activities that don’t add value
- Empower innovation by distributing control.
- Achieve durable economies of scale and scope, replacing high-overhead models
- Self-organize in scale-free distributed networks, outmaneuvering inflexible alternatives.
Community based business networks for better care.
Helping people regain health often involves many disciplines – including medical care, addiction treatment and affordable housing. Each discipline has unique requirements and ways of working.
A network model empowers a community of diverse disciplines to innovate and create better choices to meet the desired outcome for each person. Such a network focuses on ensuring service options are transparently evaluated and readily available to those who need them. Today’s reliance on large hierarchical business operations usually has one single best idea at a time, while networks create many ideas and enable us to choose what is best based on actual results.
Healthcare is a naturally collaborative profession with a strong moral drive to help people. A network model supports that inherent nature. Networks can be designed to enable practitioners to easily form unique virtual teams that serve the specific needs of each person, creating truly person-centered care.
Such scale-free networks in complex adaptive environments are agile enough to deliver economies of both scale and scope to better distribute resources and rewards to those who achieve outcomes.
Curandi: building a community network platform for outcome-based care
Curandi is dedicated to providing a network platform to support every community’s ability to organize around their shared purpose. The community’s shared purpose is implemented within the network
platform as a set of desired outcomes that apply under a wide range of conditions and circumstance. This network platform will take advantage of the community’s natural behavior to learn and adapt to each patient’s need. As performance information grows the platform enables network members to support behaviors with resources and rewards for outcomes.
This outcomes-based platform also provides a path for analytics vendors to innovate better products that deliver real-time outcome-based “in-flight instrumentation” in addition to retrospective analytics. This is an essential missing link to help practitioners and patients navigate toward better and more affordable outcomes. These outcomes become sustainable when insurers can see outcomes and support outcome based payment models. This is the same distributed empowerment today’s leading businesses take advantage of. Healthcare can replicate their growth and productivity using outcome-based business models whose distributed management uses independent lighter processes to achieve goals.
Distributed empowerment means local leaders orchestrate and manage the community network to create more and better choices for practitioners and better results for patients. It supports shared local goals, local management of outcome based decisions, local control of outcome-based contracting and reimbursement, and the ad hoc development of patient-specific virtual teams.
System efficiency comes from tuning the network which is less intrusive and much less expensive that full structural alignment.
An Oregon Pilot: Creating real value through Integration of social determinants of health
The first pilot of this 21st century approach begins January 2018. The focus will be the integration of medical care and social determinants of health (SDOH) in high-risk high-need communities.
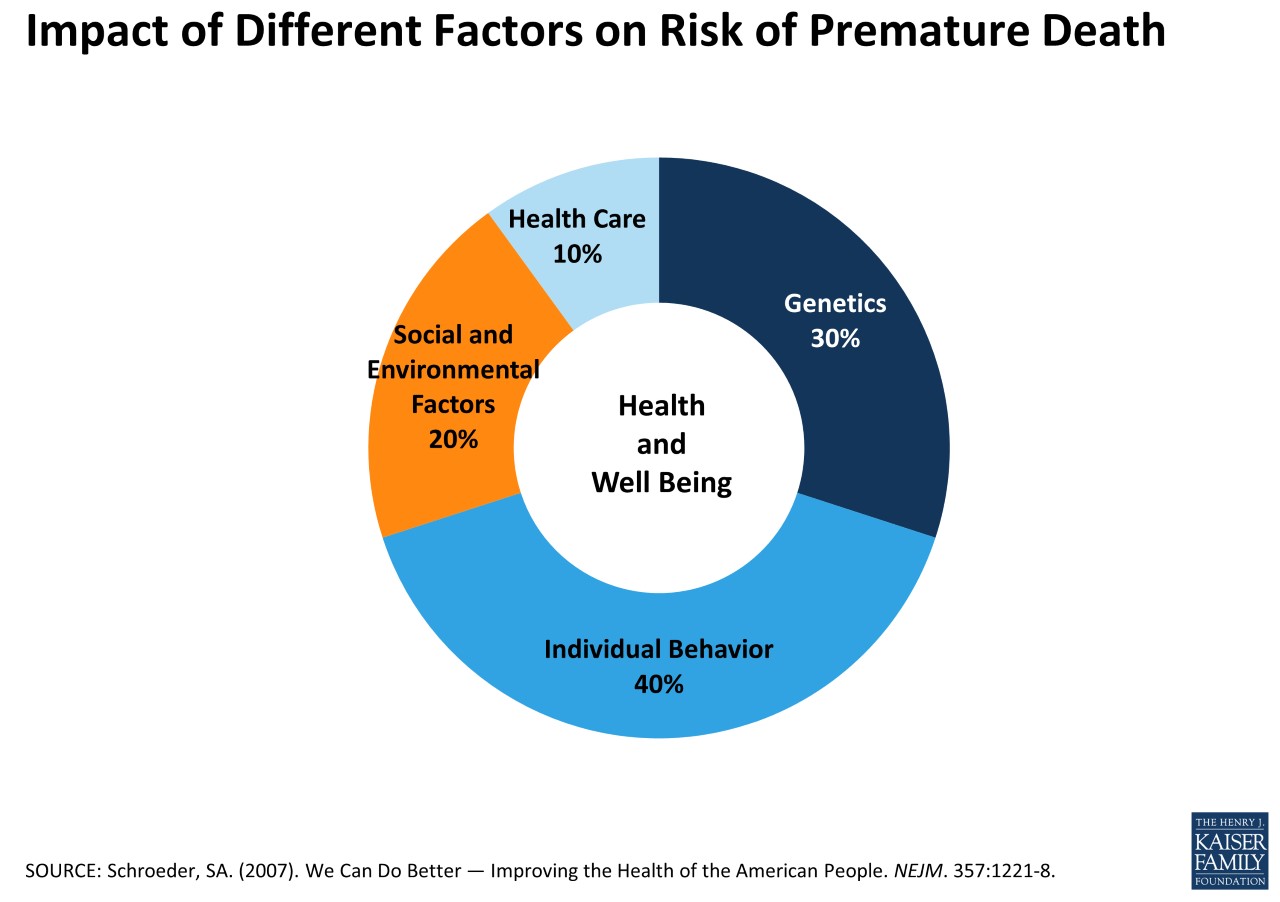
Community health is more than medical care. As figure 2 shows, the impact of social, environment and behavior may be up to six times more impactful on health than medical care. Effective integration of these into a more coherent approach is essential for long term effectiveness and affordability.
Our problem is that each discipline works in separate ways due to the different nature of each problem. Yet all are trying to achieve results that improve the lives of people and are therefore aligned at each person. This person-centered focus is a natural place for a self-organizing outcome-based network to succeed.
The pilot seeks to test a network system that:
- Enables medical care and other community health disciplines with divergent approaches to integrate efforts toward a common goal more effectively.
- Aligns care around each patient based on shared outcomes of medical, social and behavioral health organizations.
- Realize savings from addressing the whole patient within the Medicaid population within 1 to 2 years, justifying its development.
Contribute your knowledge and knowhow to developing the network model in healthcare.
- Define the core problem. Help us understand the problem better at the intersection of health and social determinants.
- Suggest a project. The underlying framework will need to be vetted in the real world.
- Accelerate technology development. The open source platform has room for developers who want to serve the greater good.