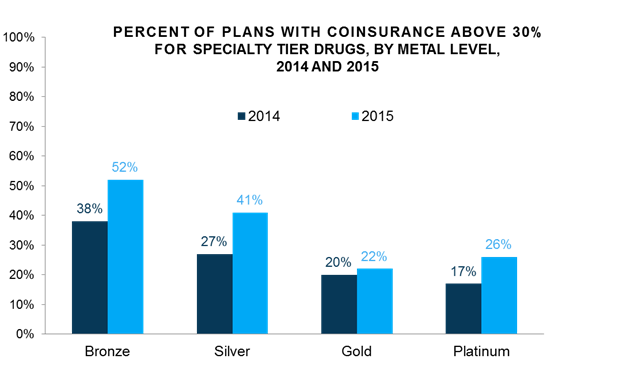
A new analysis from Avalere Health finds that patients accessing specialty medications – drugs often used to treat life-threatening illnesses, such as cancer, rheumatoid arthritis, or multiple sclerosis – through exchange plans are more likely to experience higher out-of-pocket costs in 2015 than in 2014. In particular, the incidence of plans charging coinsurance greater than 30 percent for specialty medications has increased from 27 percent of Silver plans in 2014 to 41 percent in 2015. Coinsurance is the practice of charging consumers a percentage of the total cost of the medication, as opposed to a set copayment fee. Approximately two-thirds of exchange enrollees picked Silver plans in 2014.
“Health plans continue to focus on managing drug costs to keep premiums low,” said Dan Mendelson, CEO at Avalere Health. “Competitive premiums are key to a sustainable exchange marketplace, which has led plans to pursue more significant cost-sharing. In some cases this could make it difficult for patients to afford and stay on medications.”
Overall, 80 percent of Silver plans use coinsurance for consumer cost sharing on the specialty tier. In comparison, 91 percent of Bronze, 80 percent of Gold, and 66 percent of Platinum plans charge coinsurance for specialty medications.
“Coinsurance may make medication costs unpredictable. In addition, changes in cost-sharing requirements from year-to-year may surprise some medication-dependent patients,” said Caroline Pearson, vice president at Avalere Health. “As a result, consumers who rely on specialty drugs should make sure they are evaluating their plan options in 2015. In particular, some patients may be better off paying more in monthly premiums in exchange for lower out-of-pocket costs.”
Methodology
Avalere PlanScape®, updated November, 2014. These data include the federally facilitated marketplace (FFM) landscape file, as well as data from Covered California and New York State of Health. Notably, the FFM landscape file forces plans into four tiers of data, which excludes some cost sharing detail. When plans indicated “no charge” in the HHS Landscape file, Avalere assigned the plan to $0 copayment or zero percent coinsurance depending on which cost sharing type was most prevalent for the specified benefit. For Tiers 1-3, Avalere used $0 copayment, and for Tier 4, Avalere used zero percent coinsurance.
###
If you would like to speak with an expert about these or other findings, please contact Amy Martin Vogt at 202-745-5052 or [email protected].