An analysis from Avalere shows that more health insurance plans offered through the Affordable Care Act exchanges are making some drugs used to treat complex diseases—such as HIV, cancer, and multiple sclerosis (MS)—more accessible to patients in 2016 than in previous years. Specifically, plans were less likely to place all drugs in a class on the highest cost-sharing tier.
Insurers assign drugs to a tiered structure—known as a formulary—based on out-of-pocket costs to the patients. Highest-priced medicines, which are often relied on by the most chronically ill patients, are often placed on a high formulary tier, indicating high cost-sharing for patients.
The Avalere study looks at silver-level exchange plans across 20 classes of medications. Of those, we found five classes, including drugs to treat HIV, cancer, and MS, for which some plans place all drugs in the class on the highest tier. However, the analysis finds that fewer exchange plans are doing so in 2016 than in the prior two years.
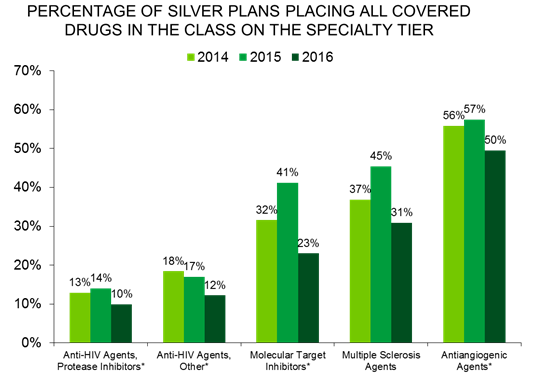
As in prior years, the class of medications most frequently subject to universal placement on the specialty tier is in the antiangiogenics class—used to treat cancer—with half of all silver plans placing all covered drugs in this class on the specialty tier in 2016. Nearly one-third of silver plans place all covered MS drugs on the specialty tier, as well; though, this rate is a drop of 14 percentage points from 2015. Additionally, the sharpest decline year-over-year (18 percentage points) is for molecular target inhibitors. For these three classes, 2016 shows a reversal of the sharp increase in this type of tiering structure that occurred between 2014 and 2015.
“The trend toward better formularies is good news for consumers,” said Caroline Pearson, senior vice president at Avalere. “Plans that place some drugs used to treat a particular condition on a lower tier may improve access to treatments and mean patients pay less out-of-pocket for their care.”
Since the launch of exchanges in 2014, patient groups and policymakers have considered whether some formulary designs might impact patients’ ability to access medications under the law. At the same time, plans continue to strive to offer innovative benefit designs that deliver low monthly premiums to consumers. CMS has issued guidance discouraging plans from placing all drugs used to treat a condition on the highest tier, without regard to the cost of the medication. However, the federal government has not yet created a tool for regulators to use to evaluate benefit designs in this regard. California also passed legislation preventing plans from placing all drugs for a condition on the highest formulary tier beginning in 2017.
“Insurance departments across the country need tools to ensure CMS’s guidance is implemented,” said Kelly Brantley, director at Avalere. “A tool that evaluates formulary tier placement could help ensure patient access.”
Avalere conducted additional analysis on the tier placement and cost sharing associated with 22 classes of medications. The full report is availablehere.
Methodology
Analysis using Avalere Health PlanScape®, a proprietary analysis of exchange plan features, updated April 2016. This analysis is based on data collected by Managed Markets Insight & Technology, LLC. The sample includes silver plans across all states. Coverage is weighted according to unique plan-state combinations. Avalere analyzed brand and generic drug coverage in a total of 20 classes, including a mix of specialty and primary care drugs.
###
To speak with an expert from Avalere about this new analysis, please contact Frank Walsh at [email protected], or 504-309-5164.
Avalere Health is a strategic advisory company whose core purpose is to create innovative solutions to complex healthcare problems. Based in Washington, D.C., the firm delivers actionable insights, business intelligence tools and custom analytics for leaders in healthcare business and policy. Avalere's experts span 230 staff drawn from Fortune 500 healthcare companies, the federal government (e.g., CMS, OMB, CBO and the Congress), top consultancies and nonprofits. The firm offers deep substance on the full range of healthcare business issues affecting the Fortune 500 healthcare companies. Avalere’s focus on strategy is supported by a rigorous, in-house analytic research group that uses public and private data to generate quantitative insight. Through events, publications and interactive programs, Avalere insights are accessible to a broad range of customers. For more information, visit avalere.com, or follow us on Twitter @avalerehealth.